By John Ford, director of the Health Equity Evidence Centre
May 2024
We have decades, if not centuries, of evidence describing health inequalities: the unfair and avoidable differences between groups. Despite this evidence, we have made little progress in tackling this complex problem. In fact, socioeconomic inequalities in life expectancy have been worsening, especially among women.
Inequalities abound across all areas of society, from income to housing and education. Health care, despite being free at the point of use in the UK, exhibits marked inequalities, particularly in primary care. The poorest areas of the UK have fewer GPs per head of population, less funding, lower patient satisfaction, and worse ratings by the Care Quality Commission.
Evidence-based approaches to tackling health inequalities
There is evidence of what works to address inequalities in primary care; however, the evidence base is disparate. There is no off-the-shelf list of effective interventions that could be implemented to address inequalities; there are rarely simple solutions for complex problems. However, there are fundamental principles that are common across the effective interventions. In 2023, we published an NIHR-funded review of what works to address inequalities in primary care. Based on a review of 325 studies, we identified five guiding principles – connected, intersectional, flexible, inclusive, and community-centred. Applying these principles is likely to address inequalities across primary care.
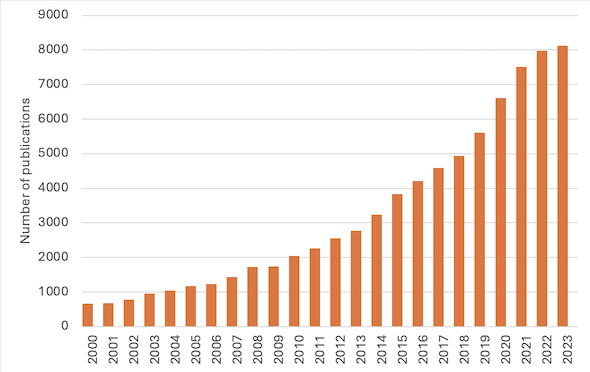
As a research team, we were delighted to publish our research but all too aware of the fundamental issues with academic literature reviews. Despite spending almost four years working on this research, from applying for funding to publishing the results, we know that the findings will go out of date. With a 280% increase over the past 10 years in primary care inequalities research publications, there is likely to be more research available since we published our study.
We are not alone; researchers are struggling to keep pace with the number of publications. Evidence suggests that reviews, when published, can be over a year out of date. If the academic world is struggling to keep up with new research, what chance do policymakers and practitioners have?
Machine learning is changing society. We’ve known about machine learning techniques for decades, but the dramatic increase in computer processing power and the large datasets available mean that we are now able to employ machine learning in new and innovative ways. One innovation is in navigating the published literature. Currently, researchers spend weeks or months manually looking through thousands and tens of thousands of research titles and abstracts. Machine learning can help.
Machine learning's role in enhancing health equity
At the Health Equity Evidence Centre, we have used our primary care inequalities review to train a machine learning algorithm. To do this, we analyse titles and abstracts of our included and excluded studies to estimate the association between common words and the likelihood of being included or excluded. We then search a database of over 250 million articles using the associations to rank articles. We then manually look through the top of the pile to pick out the most relevant articles. When we find a relevant article, we tag it with labels, and it appears in our Living Evidence Maps.
With the help of machine learning software, we only need to look through a few hundred every month, meaning that we can continually keep our evidence maps up to date, so that they are "Living." As time goes on and we make more decisions, the algorithm also improves. In addition to ranking articles, we also use citation tracking and related articles to ensure we don’t miss key studies.
Machine learning can only take us so far. We use a group of researchers to write short, accessible evidence briefs of what works to address inequalities for policymakers and practitioners. The topics we choose come straight from the NHS.
In our evidence briefs, we use transferable evidence – sometimes we don’t have enough direct research on a topic to make evidence-based recommendations, but we do have guiding principles or evidence from a comparable population. So, we logically apply this transferable evidence and communicate how confident we are using the GRADE framework.>
We believe that the days of research manually looking through thousands or tens of thousands of articles are numbered. Machine learning software is going to be a key technique as we attempt to navigate the growing body of literature. Machine learning software doesn’t do everything for us; we still need humans to select studies and synthesize them – augmentation, rather than automation.
For more information or to check out what we do, please visit our website at www.heec.co.uk.