Submitted by Anonymous on Tue, 16/09/2025 - 19:42
Mortality after emergency abdominal surgery is more than three times higher in the least developed countries compared to the most developed, according to a major new international study led by the University of Cambridge.
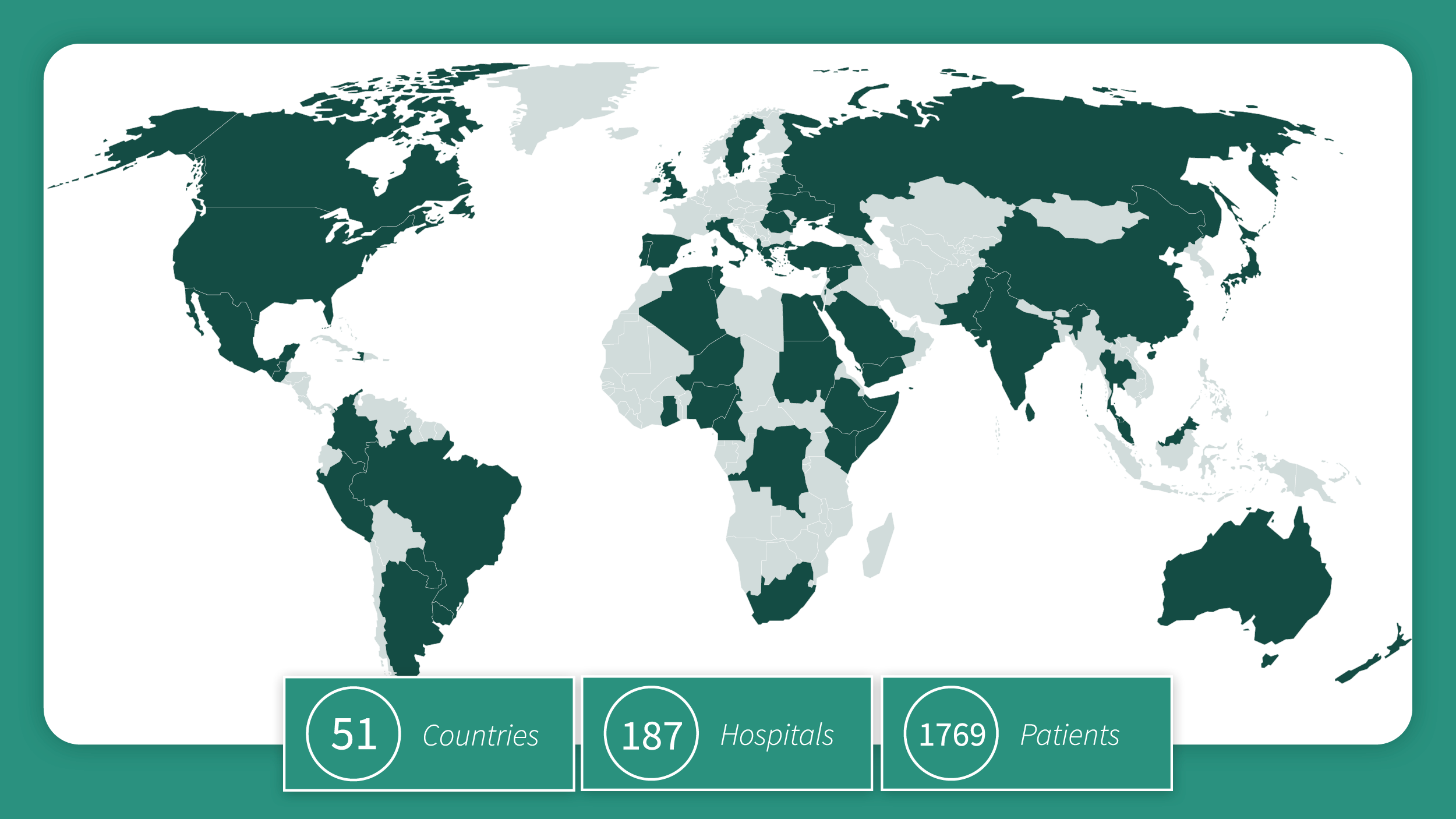
Published in The Lancet Global Health, the research analysed outcomes for 1,769 patients treated in 187 hospitals across 51 countries, ranging from conflict-affected areas such as the Occupied Palestinian Territory, Ukraine, and Sudan to well-resourced trauma centres in Europe and the United States.
It found that although overall mortality rates after surgery appeared similar at 11%, patients in the world’s least developed countries faced more than three times the risk of death compared with those in the most developed nations, as ranked by the United Nations Human Development Index (HDI).
The Global Outcomes After Laparotomy for Trauma (GOAL-Trauma) study is among the largest international investigations of trauma care to date. Dr Tom Bashford, who co-leads global health work at Cambridge Public Health, is one of the study’s senior authors.
“The GOAL-Trauma study is one of the biggest global studies of trauma care yet published," said Dr Bashford. "It represents a huge effort by a team of partners from across the world, some of whom are practising in the most extreme conditions imaginable and yet still recognise the importance of contributing to international research.”
The findings suggest that the most critically injured patients in low-HDI settings may die before reaching hospital, or that some life-threatening injuries are missed on arrival. Access to hospital care also varied widely: while over three-quarters of patients in higher-HDI countries received CT scans before surgery, fewer than one-quarter of patients in the lowest-HDI group had access to this vital diagnostic tool.
Lead investigator Dr Michael Bath, from the International Health Systems Group at the University of Cambridge, explained:
“Our findings point to a survival gap that begins before patients even reach the operating theatre. This may be because the most seriously injured die before they can access life-saving care, or because limitations in diagnosis mean their injuries go undetected.”
The study highlights the need for coordinated improvements across the entire trauma pathway – from the moment of injury through diagnosis, surgery, and recovery – to close survival gaps and ensure that critically injured patients worldwide receive the care they need.